Background: Reactivation of Cytomegalovirus (CMV) is frequent after allogeneic hematopoietic stem cell transplantation (HSCT), occurring in approximately 70% of CMV seropositive patients. CMV reactivation is associated with higher non-relapse mortality (NRM) and worse overall survival (OS), but data in patients from Latin American countries, in which seroprevalence of CMV is higher, are lacking.
Objectives: We analyzed the potential risk factors for CMV reactivation and the possible impact of CMV reactivation or primo-infection on HSCT outcomes.
Patients and Methods: We performed an observational, retrospective study in 262 consecutive adult patients who underwent HSCT between April 2007 and April 2020 in two centers. The median follow-up was 30 months.
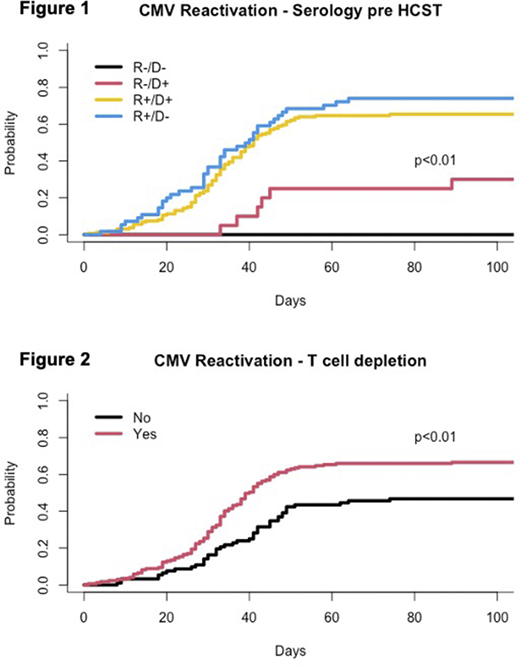
Results: The median age was 50 years (range 18 to 83), most patients (58%) were male, had acute leukemia (acute myeloid leukemia in 40%, and acute lymphoblastic leukemia in 19%), and received transplants from alternative donors (matched unrelated in 32% and haploidentical in 36%). Most transplants were from peripheral blood stem cells (73%), with reduced-intensity conditioning regimens (76%). T-cell depletion was performed in 71% (post-transplant cyclophosphamide in 40%, antithymocyte globulin - ATG in 29%, and alemtuzumab in 2%). Pre-HSCT CMV IgG serostatus of donor (D) and recipient (R) was as follows: D+/R+ in 64%, D-/R+ in 22%, D+/R- in 8%, and D-/R- in 6% only. No patient received primary CMV prophylaxis. CMV reactivations were observed in 164 patients (63%), and all received preemptive therapy at the discretion of the treating physician. The CI for CMV reactivation at 100 days (CICMV) was 74% in D-/R+, 65% in D+/R+, 30% in D+/R-, and 0% in D-/R-, p<0.01, Figure 1). The CICMV was higher in patients receiving transplants with T-cell depletion (67% vs. 47% without T-cell depletion, p<0.01), and in patients with acute graft-versus-host disease (GVHD, 91% vs. 53% without GVHD, p=0.01). By multivariate analyses, all three factors remained associated with the CMV reactivation: pre-HSCT positive CMV serostatus (Hazard Ratio - HR: 6.06; 95% Confidence Interval - 95%CI 2.76.-13.35), T-cell depletion (HR 1.65, 95%CI 1.20-2.27), and acute GVHD (HR 1.67, 95%CI 1.31-2.14). By multivariate analysis, there was no significant association between CMV reactivation and the risk of acute GVHD, chronic GVHD, mortality, relapse, or survival.
Conclusion: An increased frequency of CMV reactivation was observed in recipients with positive CMV serostatus, T-cell depletion, and acute GVHD. CMV reactivation had no significant impact on HSCT outcomes. Our findings may help to identify a group of patients who could benefit from closer monitoring and possibly primary prophylaxis with novel agents, such as letermovir.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal